| Want to send this page or a link to a friend? Click on mail at the top of this window. |
More Special Reports |
| Posted August 3, 2008 |
| National |
| Immigrants Deported, by U.S. Hospitals |
 |
|
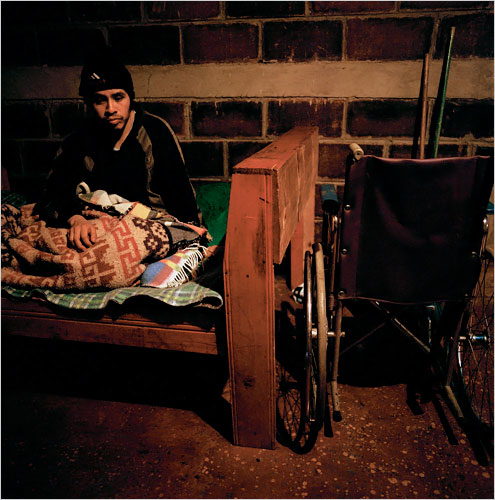
| High in the hills of Guatemala, deep inside the one-room house where he spends day and night on a twin bed, Luis Alberto Jiménez has no idea of the legal battle that swirls around him in the lowlands of Florida. Mr. Jiménez, a knit cap pulled tightly on his head, remains cheerily oblivious that he has come to represent the collision of two deeply flawed American systems, immigration and health care. Photo: Josh Haner/The New York Times More Images | |
|
|
| By DEBORAH SONTAG |
| A Life-Changing Accident |
| A Hospital's Dilemma |
| The Journey Home |
| Care in Guatemala |
| In Favor of Jiménez |
| Weighing Quality of Life |
| Wehaitians.com, the scholarly journal of democracy and human rights |
| More from wehaitians.com |